| Header | Text |
| Overview | This page provides a quick glossary of tumor terms, an overview of spinal anatomy, a description of the different types of spinal tumors, typical symptoms caused by spinal tumors, and the methods of their diagnosis and treatment.
The Spine Hospital at The Neurological Institute of New York is recognized around the world as a leader in the treatment of spinal tumors.
|
| Glossary | Benign: A benign tumor is not cancerous and will not spread to other parts of the body. Examples of spinal tumors that are usually benign include neurofibromas, schwannomas, meningiomas, ependymomas, astrocytomas, hemangioblastomas, osteosarcomas, and osteoid osteomas.
Malignant: A malignant tumor is cancerous. It will destroy nearby tissue and spread to other parts of the body. Malignant spinal tumors include chordoma, Ewing sarcoma, and occasional tumors of the types mentioned above.
Aggressive: An aggressive tumor grows or (in the case of malignant tumors) spreads quickly.
Slow-growing: A slow-growing tumor grows or spreads slowly.
Grade: A tumor’s grade is a measure of how aggressive it is likely to be. The grade is usually determined by examining tumor cells under a microscope. The resulting grade is a Roman numeral: often I (least aggressive), II, III, or IV (most aggressive). However, grading systems are different for each kind of tumor.
Metastatic: Having to do with metastasis, which is the spread of cancer from one part of the body to another.
Stage: The extent to which cancer has spread in the body. Benign tumors are not staged, because they do not spread.
Primary tumor: In metastatic disease, the primary tumor is the original tumor.
Secondary tumor: In metastatic disease, the secondary tumor represents a spread of the primary tumor. The secondary tumor contains the same cells as the original tumor (for example, lung tumor cells), but they grow in a new location (for example, in the bones of the spinal column).
|
| Spinal Anatomy | To understand spinal tumors, it helps to understand a little about basic spinal anatomy.
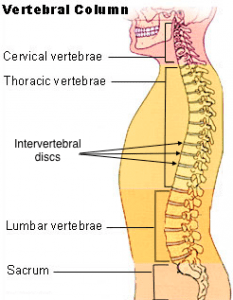
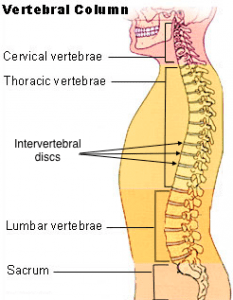
The spine is composed of many vertebrae, or individual bones of the spine, stacked one on top of another. Together, this stack forms the vertebral column. The topmost section of the vertebral column, the section in the neck, is called the cervical spine. The next section, located in the upper and mid-back, is called the thoracic spine. (The vertebrae of the thoracic spine articulate with, or form joints with, the ribs.) Below the thoracic spine is the lumbar spine, in the lower back. Finally, the sacral spine is located below the small of the back, between the hips. Sturdy intervertebral discs connect the vertebrae. The intervertebral discs act as cushions and shock absorbers between the vertebrae. Each disc is composed of a jelly-like core surrounded by a fibrous outer ring.
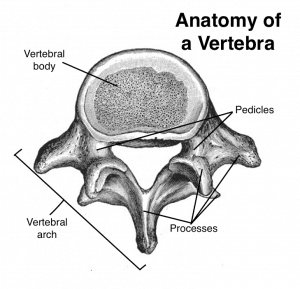
In the cervical, thoracic, and lumbar spine, all vertebrae are essentially similar. Each vertebra (the singular of vertebrae) is composed of two sections. One, the vertebral body, is a solid, cylindrical segment, shaped something like a marshmallow. It provides strength and stability to the spine. The other segment is an arch-shaped section of bone called the vertebral arch. Projecting from the back of the vertebral arch are segments of bones, called processes, that articulate with each other and provide attachment points for muscles, ligaments and tendons.
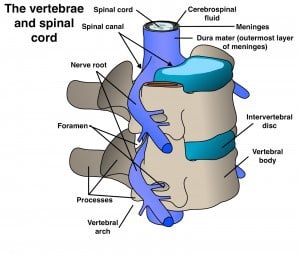
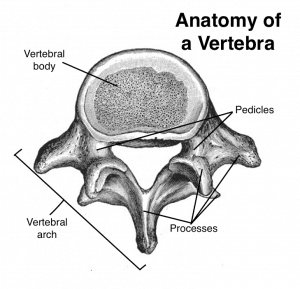 The vertebral arch is connected to the vertebral body by two small columns of bone called the pedicles. Together, the vertebral body, the pedicles, and the vertebral arch form a ring of bone around a hollow center. Stacked on top of one another in the spinal column, these rings align to form a long, well-protected channel known as the spinal canal. The vertebral arch is connected to the vertebral body by two small columns of bone called the pedicles. Together, the vertebral body, the pedicles, and the vertebral arch form a ring of bone around a hollow center. Stacked on top of one another in the spinal column, these rings align to form a long, well-protected channel known as the spinal canal.
Inside the well-protected spinal canal is the spinal cord, the delicate bundle of nerves and other tissue that connects brain and body. The spinal canal also houses the beginning of the spinal nerve roots. These are the nerves that leave the spine, exiting the spinal canal through foramen (small openings) to branch out to the body. The spinal cord and nerve roots are cushioned from the surrounding bones of the spinal canal by a liquid called the cerebrospinal fluid. Membranes called the meninges act somewhat like the casing on a sausage, wrapping up the spinal cord, the nerve roots, and the CSF inside the spinal canal. The outermost layer of the meninges is a tough tissue known as the dura mater.
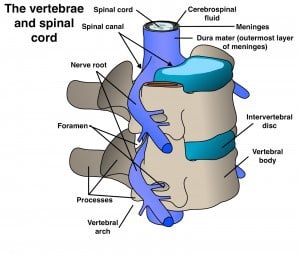
A spinal tumor is frequently classified by whether it is located inside or outside the dura mater, and whether it is located inside or outside the medulla, or substance of the spinal cord. Different types of tumors often behave differently and require varied treatments.
- Tumors located outside the dura mater are called extradural. All extradural tumors are outside the spinal cord. These tumors most often arise in the vertebrae (that is, they arise in the bones). Tumors of the vertebrae are known as vertebral column tumors. They are often metastatic tumors, but may be primary tumors of the bone.
- Tumors arising inside the dura, but outside the actual substance of the spinal cord, are termed intradural-extramedullary (inside the dura, outside the medulla). These are usually either nerve sheath tumors or meningiomas. Nerve sheath tumors arise on the nerve roots as they exit the spine, and meningiomas arise from the meninges, usually the dura.
- Tumors arising within the substance of the spinal cord itself are called intramedullary (inside the medulla). All intramedullary tumors are also inside the dura. These tumors are usually astrocytomas, ependymomas, or hemangioblastomas.
|
| Types of Spinal Tumors | Vertebral Column Tumors:
These tumors involve the bones of the vertebral column.
The majority of vertebral column tumors are metastatic. That is, the original, or primary, tumor developed in another organ and has spread to the vertebral column, usually through the bloodstream. The most common metastatic spinal tumors in women are from the breast and lung. In men, metastatic spinal tumors are most often from the prostate and lung.
Tumors arising from vertebral bone and cartilage cells also occur in the spine, although less frequently. Examples of these primary spinal column tumors include osteoid osteoma, osteoblastoma, and giant cell tumor, which are benign, and osteogenic sarcoma, chordoma, chondrosarcoma and Ewing’s sarcoma, which are malignant bone tumors.
Intradural-Extramedullary Tumors:
These tumors are located inside the dura, but outside the substance of the spinal cord.
Meningiomas and nerve sheath tumors (schwannomas and neurofibromas) comprise the overwhelming majority of this subset of spinal tumors.
Meningiomas arise from the dura mater, the thin membrane that surrounds the spinal fluid and spinal cord. Meningiomas are most common in middle-aged and older women. These tumors are usually benign.
Schwannomas and neurofibromas arise from the nerve roots that leave the spinal cord. Like meningiomas, nerve sheath tumors are usually benign.
Filum terminale ependymomas arise just below the spinal cord, in the lumbar (lower) and sacral (lowest) spinal canal. Nearly all are benign. These tumors may be large and may adhere to many nerves, making total removal sometimes difficult.
Intramedullary Tumors:
Intramedullary tumors are located inside the substance of the spinal cord.
These tumors usually arise from glia (supporting cells) within the spinal cord. Astrocytomas and ependymomas account for the majority and occur with about equal frequency, although astrocytomas are more common in children and ependymomas more common in adults.
Hemangioblastomas, tumors of blood vessels, are less common and sometimes occur in conjunction with Von Hippel Lindau disease. VHL is an inherited condition in which patients are prone to developing cysts and tumors in the kidney and other organs. Intramedullary tumors occur most often in the cervical spinal cord, or spinal cord in the neck, and are often benign.
|
| Symptoms | Spinal tumors may cause a variety of symptoms depending on their type, location, and rate of growth.
In general, the most common pattern of symptoms is pain at the tumor site in the neck or back, followed by neurological problems like weakness / numbness in the arms or legs or a change in normal bowel or bladder habits.
In patients already diagnosed with cancer of another area of the body, the new onset of spinal pain may indicate a spinal fracture caused by a metastatic tumor that has weakened a vertebra.
Tumors that arise inside the dura are usually benign and slow growing. Patients with these tumors may have pain for years before any neurological problems occur.
|
| Diagnosis | Patients who have symptoms that are suspicious for a spinal tumor should be comprehensively evaluated by a physician. Evaluation includes a complete medical history, a physical and neurological examination, and a radiographic study of the spine.
The most frequently used and most accurate radiographic study is a spinal MR (magnetic resonance) imaging scan, with and without intravenous gadolinium (a contrast-enhancing agent that makes some tumors light up brightly). These scans adequately image the spinal cord and its associated nerves. On an MRI, detail of the bony vertebral column is not as good as with CT (computed tomography – a CAT scan). However, bony detail is usually adequate with MRI, and MRI scans are capable of showing spinal cord detail, while CT scans are not.
Other radiographic studies such as CT-myelography (CAT scanning after a radiographic contrast substance is injected into the spinal fluid) or spine X-rays may also be necessary depending on the type and location of spinal tumor and its effects on the spine.
|
| Treatment | Vertebral Column Tumors:
Recall that vertebral column tumors are tumors of bone. Some vertebral column tumors are primary bone tumors, but most vertebral column tumors are metastatic tumors that have spread from cancer elsewhere in the body.
In the case of metastatic tumors, removing the spinal tumor will not cure the cancer. However, advances in treatments such as radiosurgery, separation surgery, and chemotherapy have dramatically improved the prognosis for patients with metastatic tumors. There are many treatments available to shrink the tumor or slow or stop its growth, relieve pain or neurological symptoms caused by the tumor, and maintain the stability of the spine.
Radiation therapy, either conventional or stereotactic radiosurgery, is an option that often significantly reduces spinal pain. This treatment uses highly-focused beams of radiation to disrupt tumor cells and shrink the tumor. Radiation therapy may be used to treat painful tumors if they do not compress the spinal cord or destabilize the spine.
For tumors that do compress the spinal cord or destabilize the spine, surgical treatment may be beneficial. Most benign tumors and many malignant vertebral column tumors can often be totally removed with advanced surgical techniques.
Surgery to decompress the spinal cord, called decompression surgery, consists of removing the portion of the vertebra involved with the tumor. When either decompression surgery or the tumor itself renders the spine unstable, bone grafts and metallic implants are used to restore the stability of the spine.
Intradural-Extramedullary Tumors
Recall that intradural-extramedullary tumors (mostly nerve sheath tumors and meningiomas) arise inside the dura, but outside the substance of the spinal cord.
Most intradural-extramedullary tumors are treated by total resection (total surgical removal), and patients generally report minimal or no neurological problems after surgery. However, large filum terminale ependymomas are often impossible to totally remove since they adhere to many spinal nerves. Postoperative radiation therapy may improve outcome in these cases.
Intramedullary Tumors:
Intramedullary tumors (like astrocytomas, ependymomas, and hemangioblastomas) arise within the substance of the spinal cord itself. The usual treatment for these tumors is surgical excision. The goal of surgery is to completely remove the tumor while preserving a maximum of neurological function.
For most operations on or near the spinal cord, surgeons use careful monitoring with neurophysiological techniques like SSEPs (somatosensory evoked potentials) and MEPs (motor evoked potentials). These techniques allow surgeons to monitor the spinal cord’s function during surgery, to make sure it is responding safely.
Intramedullary ependymomas and hemangioblastomas are usually well differentiated from the surrounding spinal cord and can often be removed completely. Patients may have temporary neurological problems after surgery; however, these often resolve.
By contrast, intramedullary astrocytomas may blend in with the surrounding spinal cord and can be difficult to safely remove completely. Since these tumors are usually slow growing, patients may still experience a significant benefit from less-than-total removal.
Tumors that cannot be totally removed and that show aggressive characteristics are usually treated with postoperative radiation therapy.
To see videos of the surgical removal of certain tumors, click the links below:
|
| Preparing for Your Appointment | Drs. Paul C. McCormick, Michael G. Kaiser, Peter D. Angevine, Alfred T. Ogden, Christopher E. Mandigo, Patrick C. Reid, Donald O. Quest, and Richard C.E. Anderson (Pediatric) are experts in treating spinal tumors in adults.
Dr. Richard C.E. Anderson is an expert in pediatric spinal tumors. They can also offer second opinions.
|